Introduction:
The severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2), first identified in Wuhan, China, was declared a pandemic by WHO in March 2020 due to its high transmission rate. Due to the diffuse vasculo-endothelial damage, individuals with Sickle Cell Disease (SCD) are at risk to develop severe clinical complications, if infected with coronavirus 19 (COVID-19).[1] Given this risk, a systematic evaluation of individuals with SCD presenting with COVID19 infection is paramount to identify the variable clinical manifestations and complications encountered in children and adults with SCD.
Methods:
A retrospective chart review was conducted from January to June 2020 at the Medical University of South Carolina. We included individuals with sickle cell disease of all genotypes, from 0 to 65 years of age found to be positive for COVID19 by polymerase chain reaction (PCR). Patients' past medical history, clinical presentations, admissions, treatment, complications, and mortality data were reviewed. The data was collected with REDCap@ and descriptive data analysis was conducted per SPSS@.
Results:
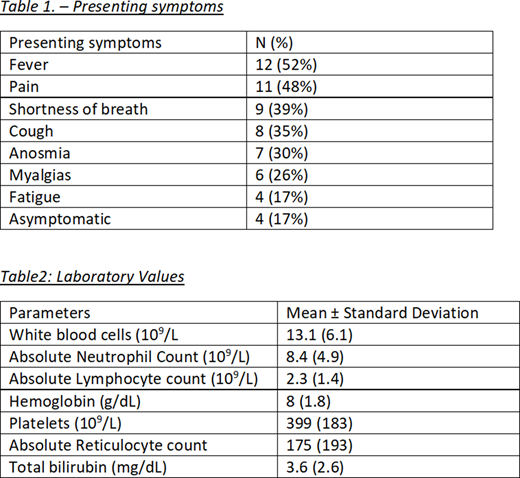
Of the identified 23 patients with SCD who tested positive for COVID during the time specified, 19 (82.6%) had Hgb SS genotype, two had Hgb SC (9%) and two Hgb Sβ+ thalassemia (9%) with similar incidence in both genders (47.8% male and 52.2 % female). All patients were African American. The mean age was 26.13+/-11.53 years. In the last three years they had admissions for pain at a mean of 4.29 +/- 5 and admissions for acute chest syndrome 1+/- 2.2. Six participants (26.1%) had history of mild asthma. Two (8.7%) had pulmonary hypertension. No participants had a history of silent stroke. One participant had history of ischemic stroke, three (13%) had history of pulmonary embolism, and six (26.1%) had deep vein thrombosis (DVT). A variable clinical presentation was noted in our population (Table 1).
Of the 23, only nine (39%) required admission of which only one met criteria for intensive care (4.3%) requiring respiratory support with high flow nasal canula. All participants recovered well with the mean length of admission 4.36+/- 3.8 days. Treatment included supportive care including transfusion support, two (8.7%) needed simple transfusion, two (8.7%) needed exchange transfusion. Regarding the laboratory values, coagulations studies were noted to be elevated among all those obtained, but overall limited values were obtained. (Table 2) Thus far no complications of stroke, thrombosis, or pulmonary emboli are noted in the patients positive for COVID in sickle cell disease at our institution. No deaths were reported.
Conclusion:
Our population reflects what has been described thus far in other cohorts regarding patient demographics, clinical presentation and evolution of disease. Missing laboratory results is most likely due to the mild severity which did not require further clinical evaluation. The absence of VTE/PE may be explained by the low rate of ICU admissions. A similar ICU admission rate of 13% in the same age group as our population was described in a study conducted in France with 83 patients. [2] Compared to a study conducted in Detroit, Michigan, our population underwent comparable rates of transfusions with 3 patients compared to 4 in our population, again most likely due to the mild severity. [3]
Our results reflect only MUSC's testing sites and we are dependent on patient's self-report which may not represent our entire population. To address this issue, as part of the Sickle Cell South Carolina network, we are partnering with two other institutions to assess SARS-Cov-2 infection in South Carolina.
SARS-CoV-2 pandemic has brought to light many disparities encountered in the American health care system. It is premature to evaluate the immediate and long-term ramifications of COVID19 in individuals with sickle cell disease, due to which we plan to continue to monitor for the next 2 years.
References
1. Hussain, F.A., et al.,COVID-19 Infection in Patients with Sickle Cell Disease.Br J Haematol, 2020.
2. Arlet, J.B., et al.,Prognosis of patients with sickle cell disease and COVID-19: a French experience.Lancet Haematol, 2020.
3. Balanchivadze, N., et al.,Impact of COVID-19 Infection on 24 Patients with Sickle Cell Disease. One Center Urban Experience, Detroit, MI, USA.Hemoglobin, 2020: p. 1-6.
Gregoski:National Institutes of Health under Grant Number UL1 TR001450:Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal